Dental Of America
- Family Dental Insurance
The American dental insurance plans are
based upon the zip code and their availability. If we are
unable to offer a dental insurance plan, we will provide a alternative dental plan, if available, and clearly state it.

Please be sure to
contact the plan dental office to confirm they are accepting new
patients and they are accepting the dental plan you have selected.
If
you have any dental insurance plan questions please feel free to
contact our office during regular business
hours. You will find our licensed insurance agents ready to assist you.
Extension of eligibility may be
made up to the age of 23 years for unmarried children who are principally
dependent upon the subscriber and are registered students in regular, full-time
attendance at an accredited school, college, or university (subscriber will be
required to submit evidence of full-time status).
 There
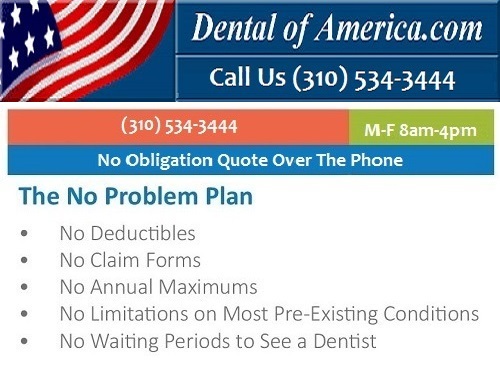
are no deductibles and no yearly limits on services, and there are no claim
forms to fill out. The dentists must meet the Plan's standard of quality and
service. All have agreed to provide dental care at a low cost available only to
its members. There is no waiting period for your dental services to begin,
pre-existing dental conditions are covered. A reminder your application must be
received by the company on or before the last day of the month prior to the
following month's coverage effective date.
There
are no deductibles and no yearly limits on services, and there are no claim
forms to fill out. The dentists must meet the Plan's standard of quality and
service. All have agreed to provide dental care at a low cost available only to
its members. There is no waiting period for your dental services to begin,
pre-existing dental conditions are covered. A reminder your application must be
received by the company on or before the last day of the month prior to the
following month's coverage effective date.
An Enrollment Application is a request for coverage, which, if approved by
California Dental Network, becomes the enrollment form used to issue an
identification card and Combined Evidence of Coverage and Disclosure Form. All
benefits, limitations and exclusions are stated in full in the Combined Evidence
of Coverage and Disclosure Form which is provided
 when
coverage becomes effective. Members will have 30 days from receipt of the
Combined Evidence of Coverage and Disclosure Form to cancel their enrollment and
receive a full refund of their premiums if they have not utilized the Plan. You
may obtain a copy of the Combined Evidence of Coverage and Disclosure Form from
their Corporate Office before you enroll.
when
coverage becomes effective. Members will have 30 days from receipt of the
Combined Evidence of Coverage and Disclosure Form to cancel their enrollment and
receive a full refund of their premiums if they have not utilized the Plan. You
may obtain a copy of the Combined Evidence of Coverage and Disclosure Form from
their Corporate Office before you enroll.
Limitations (1) Prophylaxis (cleaning) is limited to once every six months. (2)
Fluoride treatment is covered once every 12 months for Members up to age 14. (3)
Bitewing x-rays are limited to one series of four films every 12 months. (4)
Full mouth x-rays are limited to once every 24 months. (5) Sealants are covered
for Members up to the age of 14 and are limited to permanent first and second
molars. (6) Periodontal treatments (subgingival curettage and root planning)
 are
limited to one treatment per quadrant in any 12-month period. (7) Fixed
bridgework will be covered only when a partial cannot satisfactorily restore the
case.(8) Replacement of partial dentures is limited to once every five years.
(9) Full upper and/or lower dentures are not to exceed one each in any five-year
period. (10) Denture relines are limited to one per arch in any 12-month period.
are
limited to one treatment per quadrant in any 12-month period. (7) Fixed
bridgework will be covered only when a partial cannot satisfactorily restore the
case.(8) Replacement of partial dentures is limited to once every five years.
(9) Full upper and/or lower dentures are not to exceed one each in any five-year
period. (10) Denture relines are limited to one per arch in any 12-month period.
Exclusions (1) General anesthesia, analgesia (nitrous oxide), intravenous
sedation, or the services of an anesthesiologist. (2) Treatment of fractures or
dislocations; congenital malformations; malignancies, cysts, or neoplasms; or
Temporomandibular Joint Syndrome (TMJ). (3) Extractions or x-rays for
orthodontic purposes. (4) Prescription drugs and over the counter drugs. (5) Any
services involving implants or experimental procedures. (6) Any procedures
performed for cosmetic, elective or aesthetic purposes. (7) Any procedure to
replace or
 stabilize
tooth structure lost by attrition, abrasion, erosion or grinding.
stabilize
tooth structure lost by attrition, abrasion, erosion or grinding.
Not all general dentists are
capable of performing each of the services listed herein and, based upon the
Memberís condition, certain procedures may not be within the scope of practice
or ability of a general dentist. In such cases, the general dentist will refer
the Member to a California
Dental Network participating dental specialist, who will give the Member a 30%
discount from their regular fees during the first year of enrollment, and a 50%
discount thereafter, for up to $1,000 in services per year. The ratio of premium
costs to health services paid, for plan contracts with individuals and groups of
25 or fewer members, during the preceding fiscal year was 0%. * UCR means the
dentistís or specialistís Usual, Customary & Reasonable fees. # Member is
responsible for the payment shown plus the actual lab cost of gold.
Orthodontists may charge Members additional fees for costs of cases over 24
months, based on the differences in UCR fees for the needed treatment periods
less the UCR fees for a 24-month treatment period.

